Penetrance and pleiotropy of polygenic risk scores for schizophrenia in 90,000 patients across three healthcare systems
 Associations with genetic risk for schizophrenia across hospital systems
Associations with genetic risk for schizophrenia across hospital systems
Penetrance and pleiotropy of polygenic risk scores for schizophrenia in 90,000 patients across three healthcare systems
Abstract
BACKGROUND: Individuals at high risk schizophrenia may benefit from early intervention but few validated risk predictors are available. Genetic profiling is one approach to risk stratification that has been extensively validated in research cohorts, but its utility in clinical settings remains largely unexplored. Moreover, the broad health consequences of a high genetic risk of schizophrenia are poorly understood, despite being highly relevant to treatment decisions.
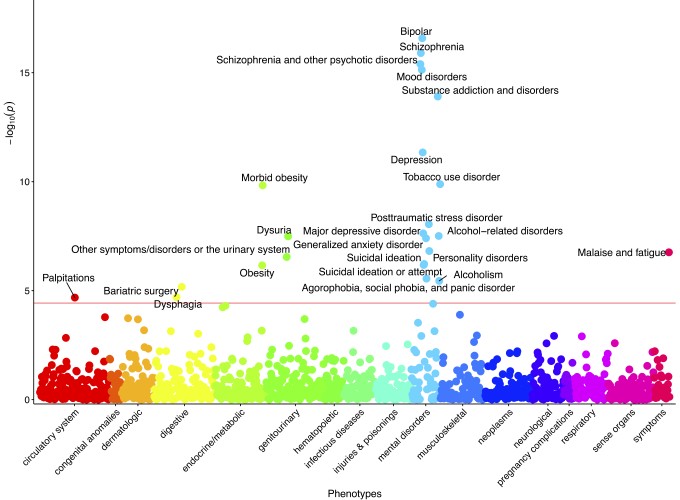
METHODS: We used electronic health records of 91,980 patients from three large healthcare systems to evaluate the penetrance and pleiotropy of genetic risk for schizophrenia. Polygenic risk scores (PRSs) for schizophrenia were calculated from meta-analysis summary statistics and tested for association with schizophrenia diagnostic codes and 1338 code-defined disease categories in a phenome-wide association study. Effect estimates were meta-analyzed across sites, and follow-up analyses evaluated the effect of a schizophrenia diagnosis.
RESULTS: PRSs were robustly associated with schizophrenia (odds ratio per standard deviation increase in PRS = 1.65 [95% confidence interval (CI), 1.5-1.8], p = 1.25 x 10-16) and patients in the highest risk decile of the PRS distribution had a four-fold increased odds of schizophrenia compared to those in the bottom decile (95% CI, 2.4-6.5, p = 4.43 x 10-8). PRSs were also associated with other psychiatric phenotypes, including anxiety disorders, bipolar disorder, depression, substance use disorders, personality disorders, and suicidal behavior. Non-psychiatric associations included heart palpitations, urinary syndromes, obesity, and nonspecific somatic symptoms. Most associations remained significant when conditioning on a diagnosis of schizophrenia, indicating genetic pleiotropy.
CONCLUSIONS: We demonstrate that an available measure of genetic risk for schizophrenia is robustly associated with schizophrenia in healthcare settings and has pleiotropic effects on related psychiatric disorders as well as other medical symptoms and syndromes. Our results provide an initial indication of the opportunities and limitations that may arise with the future application of PRS testing in healthcare systems.
More detail can easily be written here using Markdown and $\rm \LaTeX$ math code.